General
There are multiple types of biomarkers, some are used in a diagnostic context, others to monitor disease, analyse risk, determine prognosis, or are targeted to treat the disease[1]. Biomarkers can also be composite or digital, such as sensors[2]. These facilitate continuous tracking rather than providing a snapshot of the state of the body at a certain point in time[3]. An example of a digital biomarker would be using wearable electronic devices to collect data during a walk test about exercise tolerance[4]. The term biomarker may be unfamiliar to you, but many have heard of cholesterol levels being able to provide information about heart health or PSA screenings being done for prostate cancer. These are two examples of many depicting biomarker usage in healthcare. This usage is a two step process: first the biomarker must be detected through testing, then it can be targeted therapeutically.
Detection: Cancer Biomarkers Sample Types
[5][6][7][8]
Below are the most to least common types of samples used to perform biomarker testing and identify cancer-associated biomarkers.
Most to Least Common Sample Types used in Biomarker Testing
| Most Common | Common | Least Common |
|
|
|
Comparison of Liquid vs Tissue Biopsy
[9]
| Biopsy | Advantages | Disadvantages |
| Liquid |
|
|
| Tissue |
|
|
The above information is from the Canadian Urologists Association.
Tumour Tests
Tests can be performed on tumour tissue scanning for biomarkers that are associated with certain cancers. Tissue samples are collected by doing a biopsy in a lab or at a hospital. The biomarkers being tested for are typically regular components of the cell, the difference is in the level of that component (usually more or less than usual). These altered levels are either a direct result of the tumour or the body’s response to it. Tumour tests help with cancer diagnosis, quantifying cancer spread, treatment plan, and monitoring whether the treatment is successful. It’s important to keep in mind that a tumour test that involves sequencing can’t confirm whether a biomarker was inherited or not. A sample must be taken from another site of the body for that to confirm that the mutation
Known Cancer-Associated Biomarkers Identified Through Tumour Tissue/Bone Marrow and Their Applications
Cancer Type:
- Non-small cell lung cancer
- Anaplastic large cell lymphoma
- Histiocytosis
Application:
- Helps determine which treatment approach to take
- Helps analyze prognosis
Cancer Type: B-cell lymphoma
Application:
- Helps in diagnosis
- Evaluate how effective the treatment is
- Check for reoccurance
Cancer Type:
- Lymphomas
- Leukemias
Application:
- Helps in diagnosis
- Helps plan therapy
Cancer Type:
- Chronic myeloid leukemia
- Acute lymphoblastic leukemia
- Acute myelogenous leukemia
Application:
- Helps confirm diagnosis
- Predict response to targeted therapy
- Determine treatment
- Monitor disease status
Cancer Type:
- Cutaneous melanoma
- Erdheim-Chester disease
- Langerhans cells histiocytosis
- CRC
- Non-small cell lung cancer
Application: Helps determine the appropriate treatment for the patient
Cancer Type:
- Ovarian cancer
- Breast cancer
- Prostate cancer
- Pancreatic cancer
- Melanoma
Application: Helps determine treatment
Cancer Type:
- B-cell lymphomas
- Leukemias
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type:
- B-cell lymphomas
- Leukemias
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type:
- Classic Hodgkin lymphoma
- B-cell lymphoma
- T-cell lymphoma
Application: Helps determine treatment
Cancer Type:
- Gastrointestinal stromal tumour
- Mucosal melanoma
- Acute myeloid leukemia
- Mast cell disease
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type:
- Lymphoma
- Myeloma
Application: Helps in diagnosis
Cancer Type: Non-small cell lung cancer
Application:
- Helps determine treatment
- Helps analyse prognosis
Cancer Type: Breast cancer
Application: Helps determine treatment
Cancer Type: Bladder cancer
Application: Helps determine treatment
Cancer Type:
- Breast
- Ovarian
- Bladder
- Pancreatic
- Stomach Cancers
Application: Helps determine treatment
Cancer Type: Acute myeloid leukemia
Application: Helps determine treatment
Cancer Type: Lymphoma
Application: Helps in diagnosis
Cancer Type: Certain types of leukemia
Application: Helps in diagnosis
Cancer Type:
- Colorectal cancer
- Non-small cell lung cancer
Application: Helps determine treatment
Cancer Type:
- Colorectal cancer
- Other solid tumours
- Endometrial
- gastric
Application:
- Guides treatment
- Helps identify those at high risk of certain cancer-predisposition syndromes
More info on MSI here
Cancer Type:
- Lymphomas
- Leukemias
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type:
- Lymphomas
- Waldenström macroglobulinemia
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type: Any solid tumour
Application: Helps determine treatment
Cancer Type: Acute promyelocytic leukemia
Application:
- Helps in diagnosis
- Predicting response to all-transretinoic acid or arsenic trioxide therapy
- Assess effectiveness of therapy
- Monitor minimal residual disease
- Predict early relapse
Cancer Type:
- Non small cell lung cancer
- Liver cancer
- Stomach cancer
- Gastroesophageal junction cancer
- Classical Hodgkin lymphoma
- Other aggressive lymphoma subtypes
Application: Helps determine treatment
Cancer Type: Non small cell lung cancer
Application: Helps determine treatment
Cancer Type: Neuroendocrine tumours affecting the pancreas or gastrointestinal tract
Application: Helps determine treatment
Cancer Type: T-cell lymphoma
Application: Helps in diagnosis; sometimes to detect and evaluate residual disease
Cancer Type:
- Leukemia
- Lymphoma
Application: Helps in diagnosis
Cancer Type: Breast cancer
Application:
- Helps determine the aggressiveness of the cancer
- Guides treatment
Cancer Type: Glioblastoma
Application: Drug response to chemotherapy
Cancer Type: Lynch syndrome
Application: Informs treatment decision
Tumour Marker Tests in Common Use was originally published by the National Cancer Institute.
Blood Tests
[13]
When a blood test is performed, we can use different parts of the blood to search for biomarkers. To our eyes, blood just looks like a red fluid but it is actually a blend of white blood cells, plasma, serum and possibly a small amount of tumour cells or DNA that have been released from solid tumours into the blood. These tumour cells found in the blood (which you may see referred to as “circulating tumour cells”) are often a sign that the cancer is using the blood as a method of transportation to another site of the body; in other words it’s metastasizing. Due to that knowledge, we use these circulating tumour cells as a biomarker in metastatic prostate, breast and colorectal cancer as a sign that the cancer is spreading.
Known Cancer-Associated Biomarkers Identified Through Blood Samples and Their Applications [14]
Cancer Type:
- Liver cancer
- Germ cell (inherited) tumours
Application:
- Helps diagnose liver cancer
- Track how well someone is responding to treatment including hereditary tumours
- Assess the stage and likely outcome of the cancer
Cancer Type: B-cell lymphoma
Application:
- Helps in diagnosis
- Evaluate how effective the treatment is
- Check for reoccurance
Cancer Type:
- Lymphomas
- Leukemias
Application:
- Helps in diagnosis
- Helps plan therapy
Cancer Type:
- Chronic myeloid leukemia
- Acute lymphoblastic leukemia
- Acute myelogenous leukemia
Application:
- Helps confirm diagnosis
- Predict response to targeted therapy
- Determine treatment
- Monitor disease status
Cancer Type:
- Multiple myeloma
- Chronic lymphocytic leukemia
- Some lymphomas
Application:
- Helps determine prognosis
- Allows us to follow the response to treatment
Cancer Type:
- Choriocarcinoma
- Germ cell (inherited) tumours
Application:
- Helps assess stage of cancer
- Helps determine prognosis
- Allows us to access the response to treatment
Cancer Type:
- Ovarian cancer
- Breast cancer
- Pancreatic cancer
- Prostate cancer
- Melanoma
Application:
- Helps determine treatment
- Encourages more frequent screening if the person has the gene but doesn’t have cancer yet since it’s hereditary
Cancer Type: Breast cancer
Application:
- Helps assess whether the treatment is working
- Helps identify is cancer has recurred
Cancer Type:
- Pancreatic cancer
- Gallbladder cancer
- Bile duct cancer
- Gastric cancers
Application: Helps assess whether the treatment is working
Cancer Type: Ovarian cancer
Application:
- Helps diagnose this cancer type
- Assess whether the treatment is working
- Identify if the cancer has recurred
Cancer Type: Breast cancer
Application:
- Helps detect metastasis
- Identify if the cancer has recurred
Cancer Type: Medullary thyroid cancer
Application:
- Helps diagnose this cancer type
- Helps check whether treatment is working
- Assess recurrence
Cancer Type:
- Colorectal cancer
- Some other cancers
Application:
- Helps observe how effective the treatment is
- Identify is the cancer has recurred spread
Cancer Type:
- B-cell lymphomas
- Leukemias
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type: Non-Hodgkin lymphoma
Application: Helps determine treatment
Cancer Type:
- B-cell lymphomas
- Leukemias
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type: Non-Hodgkin (T-cell) lymphoma
Application: Helps determine treatment
Cancer Type: Acute myeloid leukemia
Application: Helps determine treatment
Cancer Type: Neuroendocrine tumours
Application:
- Helps in diagnosis
- Helps check whether the treatment is working
- Identify if the cancer has recurred
Cancer Type: Chronic lymphocytic leukemia
Application: Helps determine treatment
Cancer Type:
- Metastatic breast cancer
- Metastatic prostate cancer
- Metastatic Colorectal cancer
Application:
- Helps inform clinical decision making
- Assess prognosis
Cancer Type:
- Gastrointestinal stromal tumour
- Mucosal melanoma
- Acute myeloid leukemia
- Mast cell disease
Application:
- Helps in diagnosis
- Helps determine treatment
Cancer Type: Lung cancer
Application: Help monitor for recurrence of the cancer
Cancer Type: Hepatocellular carcinoma
Application:
- Helps monitor the effectiveness of treatment
- Helps monitor for recurrence of the cancer
Cancer Type:
- Breast cancer
- Colorectal cancer
- Gastric cancer
- Pancreatic cancer
Application: Helps predict the risk of a toxic reaction to 5-fluorouracil-5 therapy
Cancer Type: Acute myeloid leukemia
Application: Helps determine treatment
Cancer Type: Gastrin-producing tumor (gastrinoma)
Application:
- Helps in diagnosis
- Helps monitor the effectiveness of treatment
- Helps monitor for recurrence
Cancer Type: Ovarian cancer
Application:
- Helps determine/plan treatment
- Assess disease progression
- Monitor for recurrence
Cancer Type: Acute myeloid leukemia
Application: Helps determine treatment
Cancer Type:
- Multiple myeloma
- Waldenström macroglobulinemia
Application:
- Helps in diagnosis
- Assess response to treatment
- Monitor for recurrence
Cancer Type: Certain types of leukemia
Application: Helps in diagnosis
Cancer Type:
- Germ cell (inherited) tumours
- Lymphoma
- Leukemia
- Melanoma
- Neuroblastoma
Application:
- Helps assess stage of the cancer
- Assess prognosis
- Helps evaluate response to treatment
Cancer Type: Leukemia
Application: Helps in diagnosis
Cancer Type:
- Small cell lung cancer
- Neuroblastoma
Application:
- Helps in diagnosis
- Assess response to treatment
Cancer Type: Acute promyelocytic leukemia
Application:
- Helps in diagnosis
- Predicting response to all-transretinoic acid or arsenic trioxide therapy
- Assess effectiveness of therapy
- Monitor minimal residual disease
- Predict early relapse
Cancer Type: Prostate cancer
Application:
- Helps in diagnosis
- Assess the response to treatment
- Monitor for recurrence
Cancer Type: Metastatic prostate cancer
Application: Helps in diagnosis of poorly differentiated carcinomas
Cancer Type: Mesothelioma
Application: Helps monitor the progression or recurrence
Cancer Type: T-cell lymphoma
Application: Helps in diagnosis; sometimes to detect and evaluate residual disease
Cancer Type:
- Leukemia
- Lymphoma
Application: Helps in diagnosis
Cancer Type: Thyroid cancer
Application:
- Helps evaluate response to treatment
- Monitor for recurrence
Tumour Marker Tests in Common Use was originally published by the National Cancer Institute
Urine Tests
Urine tests are often used to detect biomarkers associated with bladder or prostate cancer. This can be helpful for diagnosis as well as surveillance of pre-existing cancer and could likely reduce the number of unnecessary cystoscopies (the procedure where a thin tube with an attached camera is inserted into the bladder) [15].
To read more about using urine tests to analyze DNA check out this article.
Known Cancer-Associated Biomarkers Identified Through Urine Samples and Their Applications [16] [16]
Cancer Type:
- Multiple myeloma
- Chronic lymphocytic leukemia
- Some lymphomas
Application:
- Helps determine prognosis
- Allows us to follow the response to treatment
Cancer Type:
- Choriocarcinoma
- Germ cell (inherited) tumours
Application:
- Helps assess stage of cancer
- Helps determine prognosis
- Allows us to access the response to treatment
Cancer Type:
- Bladder cancer
- Cancer of the Kidney
- Cancer of the Ureter
Application: Allows for the surveillance of the cells and cystoscopy of patients who are already known to have bladder cancer
Cancer Type: Bladder Cancer
Application: Helps monitor for tumour recurrence
Cancer Type: Bladder cancer
Application:
- Helps monitor progression
- Helps confirm whether the treatment is working
Cancer Type: Carcinoid tumours
Application:
- Helps determine diagnosis
- Monitor disease
Cancer Type:
- Multiple myeloma
- Waldenström macroglobulinemia
Application:
- Helps in diagnosis
- Assess response to treatment
- Monitor for recurrence
Cancer Type: Bladder cancer
Application: Helps monitor response to treatment
Cancer Type: Prostate cancer
Application: Helps determine need for repeating biopsy after a negative biopsy
Cancer Type: Colorectal cancer
Application: Helps in diagnosis
Tumour Marker Tests in Common Use was originally published by the National Cancer Institute
Stool tests
Stool samples are typically collected to perform screenings for colorectal cancer. Tumours will release small amounts of blood into the stool, so that is one of the things these tests look for as well as polyps [17]. However, distinguishing between colorectal cancer and hemorrhoids can be difficult since they would both yield similar test results. Stool samples can also be used to detect colorectal cancer biomarkers, in this case there’s not that same issue of it potentially being hemorrhoids [18]. Beyond those two approaches, stool samples can be used to analyze the microorganisms in a person’s body, which are used as a biomarker and give us information on how someone will respond to treatment[19][20].
Known Cancer-Associated Biomarkers Identified Through Stool and Their Applications [21]
| Biomarker/Gene | Cancer Type | Application |
| NDRG4 and BMP3 methylated promoter
Epigenetic change |
|
|
Tumour Marker Tests in Common Use was originally published by the National Cancer Institute
Cerebrospinal Fluid Tests
These tests are done to analyze proteins in the cerebrospinal fluid to see if there are altered levels which may indicate cancer. An example of a biomarker found in cerebrospinal fluid is listed below.
Known Cancer-Associated Biomarkers Identified Through Cerebrospinal Fluid and Their Applications[22]
| Biomarker/Gene | Cancer Type | Application |
| Beta-2-microglobulin (B2M) |
|
|
Tumour Marker Tests in Common Use was originally published by the National Cancer Institute
Saliva/Buccal Swab Tests
These types of tests are often done to look for hereditary mistakes in the DNA, but it can also look for proteins and other components of the cell.
Known Cancer-Associated Biomarkers Identified Through Saliva/Buccal Swabs and Their Applications [23]
| Biomarker/Gene | Cancer Type | Application |
| UGT1A1*28 variant homozygosity |
|
|
Tumour Marker Tests in Common Use was originally published by the National Cancer Institute
Risks with Hereditary Germline Mutations
On the topic of biomarkers, there are a number of genetic biomarkers that are not only known to be associated with certain types of cancers, but that are also heritable which you may see being referred to as “germline mutations”. These can be passed down from parent to child, meaning the biomarker discovered is in every cell of your body, not just the cancerous tumour. Many of the known heritable biomarkers are listed below with links to more information about each from the FORCE website.
Other BRCA resources
“What are the Risks with BRCA Mutation” Handout
If a biomarker known to be associated with a certain cancer type is discovered during a genetic test, there are varying levels of cancer risk depending on the identity of the biomarker. The different levels of risk tied to each are outlined in this handout.
Risk of Cancer by Type Amongst the General Population vs People with the BRCA1 & 2 Biomarkers [24]
| Cancer Type | General Population Risk (%) | Risk of Cancer | |
| BRCA1 (%) | BRCA2 (%) | ||
| Breast | 12 | 55-72 (by age 70) | 45-69 |
| Ovarian | 1-2 | 39-44 | 11-17 |
| Male breast | 0.1 | 1-2 | 6-8 |
| Prostate | 6 (by age 69) | 21 (by age 75);
29 (by age 85) |
27 (by age 75)
60 (by age 85) |
| Pancreatic | 0.5 | 1-3 | 3-5 (by age 70) |
| Melanoma | 1.6 | Elevated risk | |
*Note all the linked biomarker information is from Facing Hereditary Cancer EMPOWERED
 To learn more about biomarkers and the cancers/tumour types they are associated with visit McGill’s MIPOGG tool at this link and scroll to the resources section.
To learn more about biomarkers and the cancers/tumour types they are associated with visit McGill’s MIPOGG tool at this link and scroll to the resources section.
At this link you will find a table outlining the connection between certain biomarkers and various associated cancers. Multi-cancer panel: genes and associated cancers
Cancer-specific
Current Biomarkers
CCRAN Biomarkers Conference 2025
Generating a Cost-Benefit Analysis to Help Support Access to Comprehensive Genomic Profiling (CGP) for Five Metastatic Cancers in Canada: Helping to Ensure CGP Becomes a Standard of Care in Canada!
Eddy Nason, MPhil, B.Sc., Director, Health, Conference Board of Canada
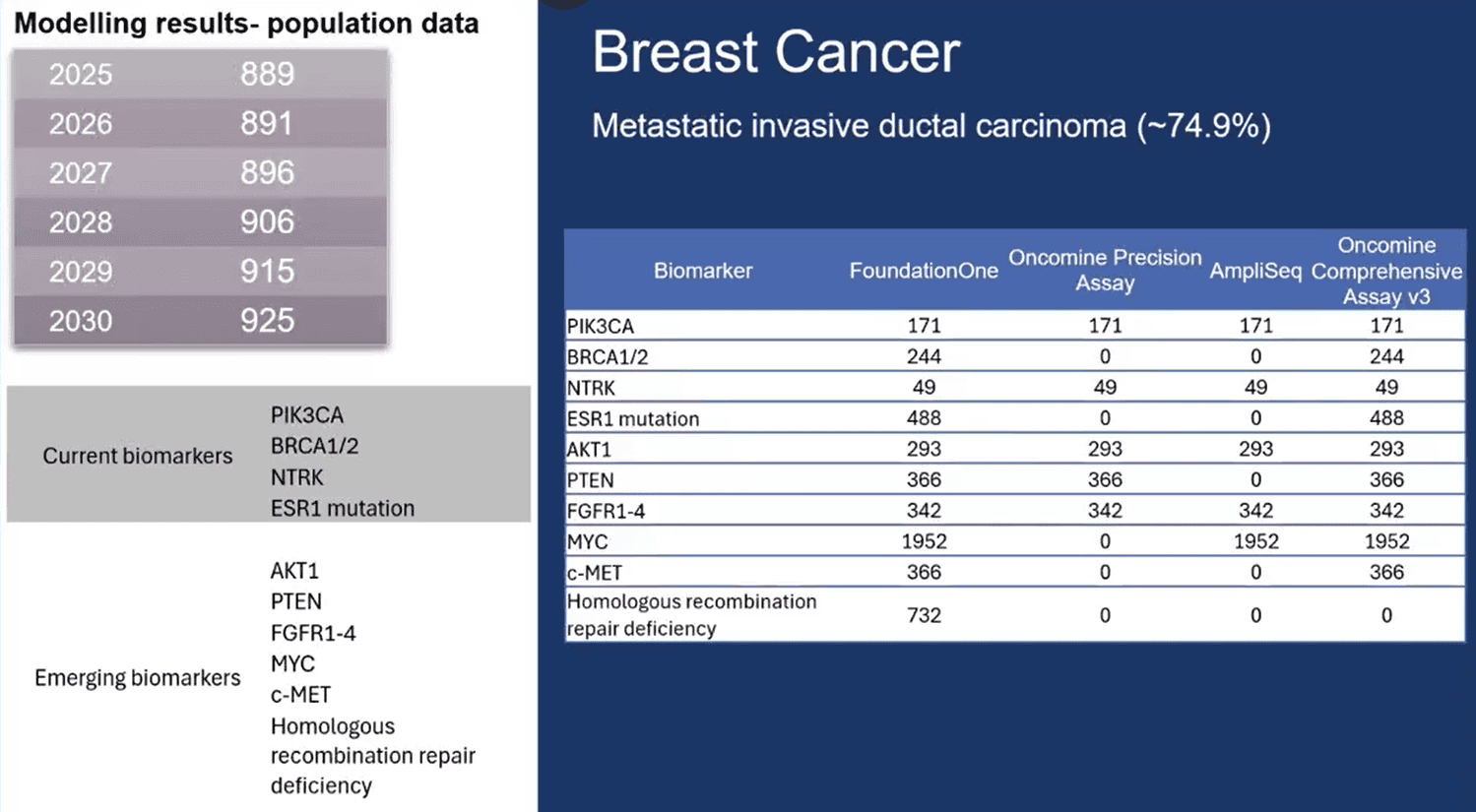
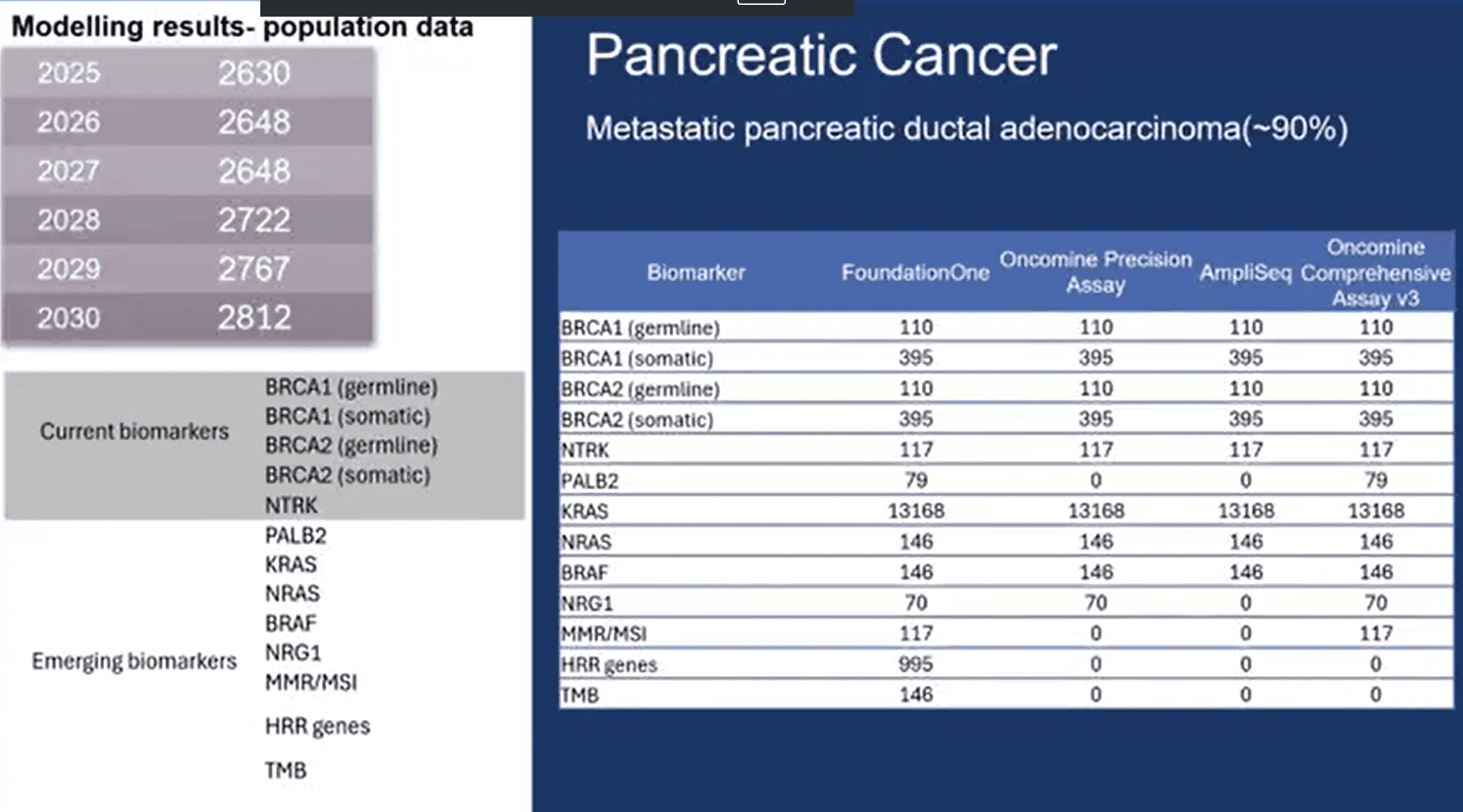
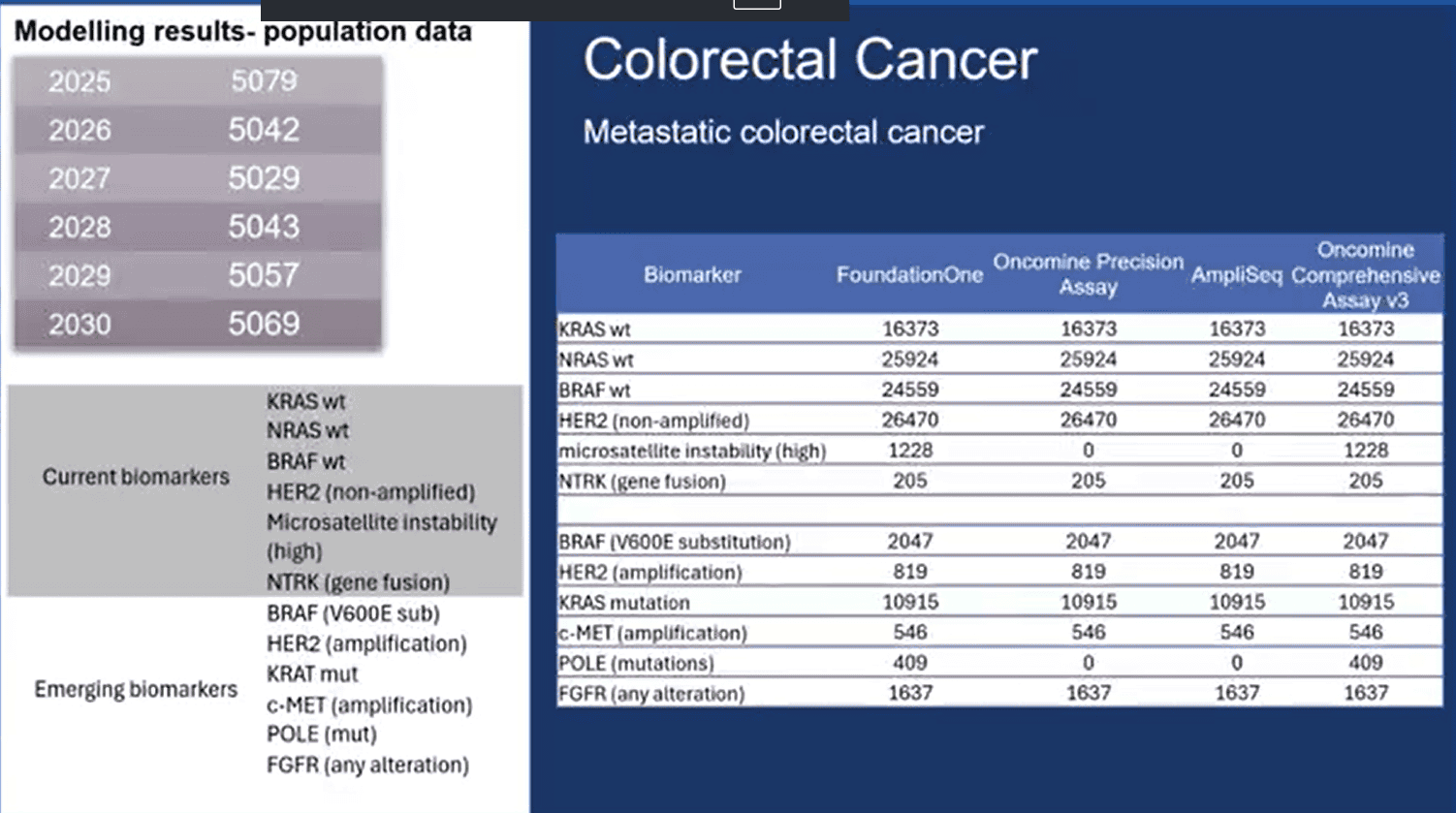
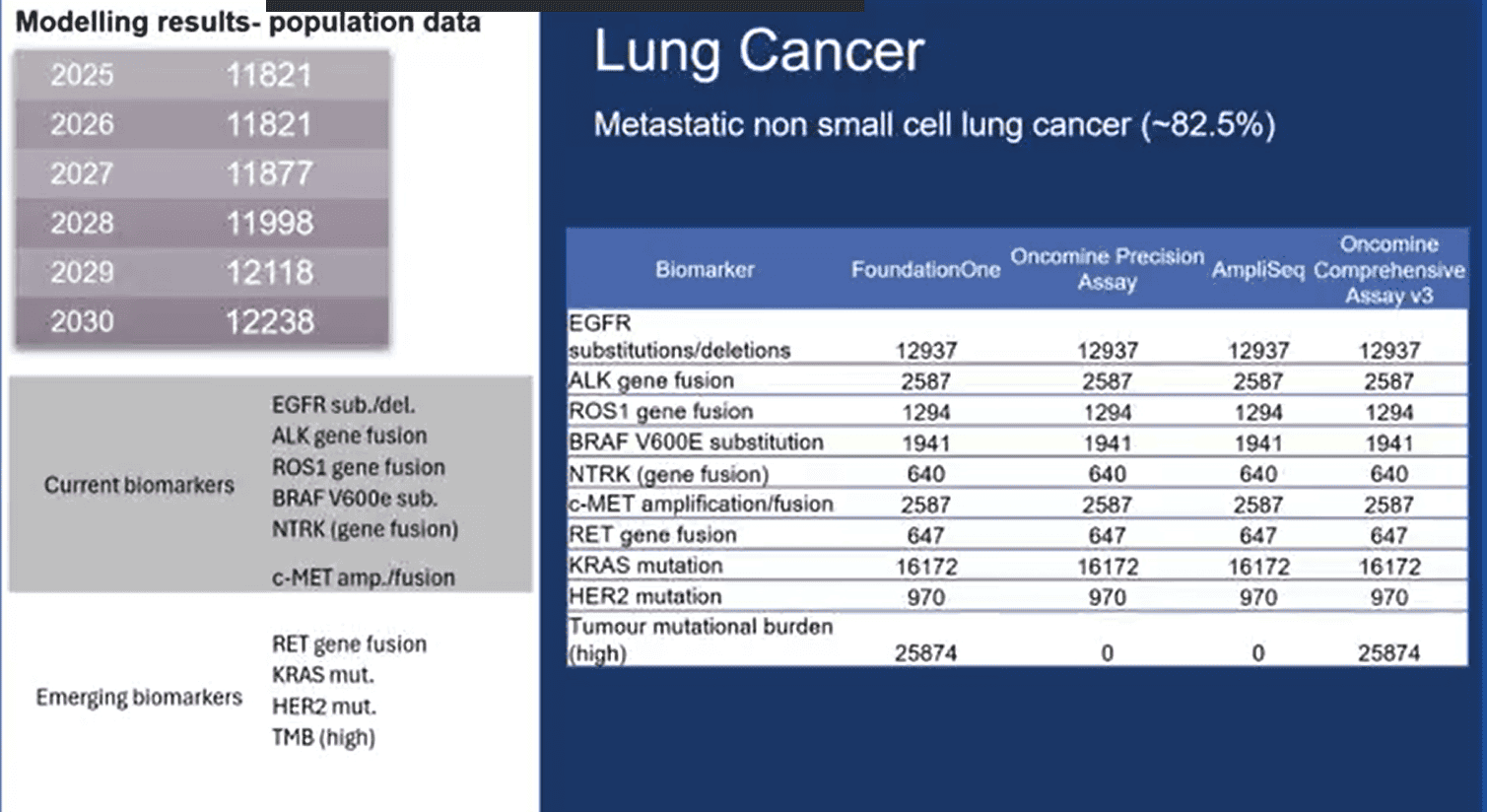
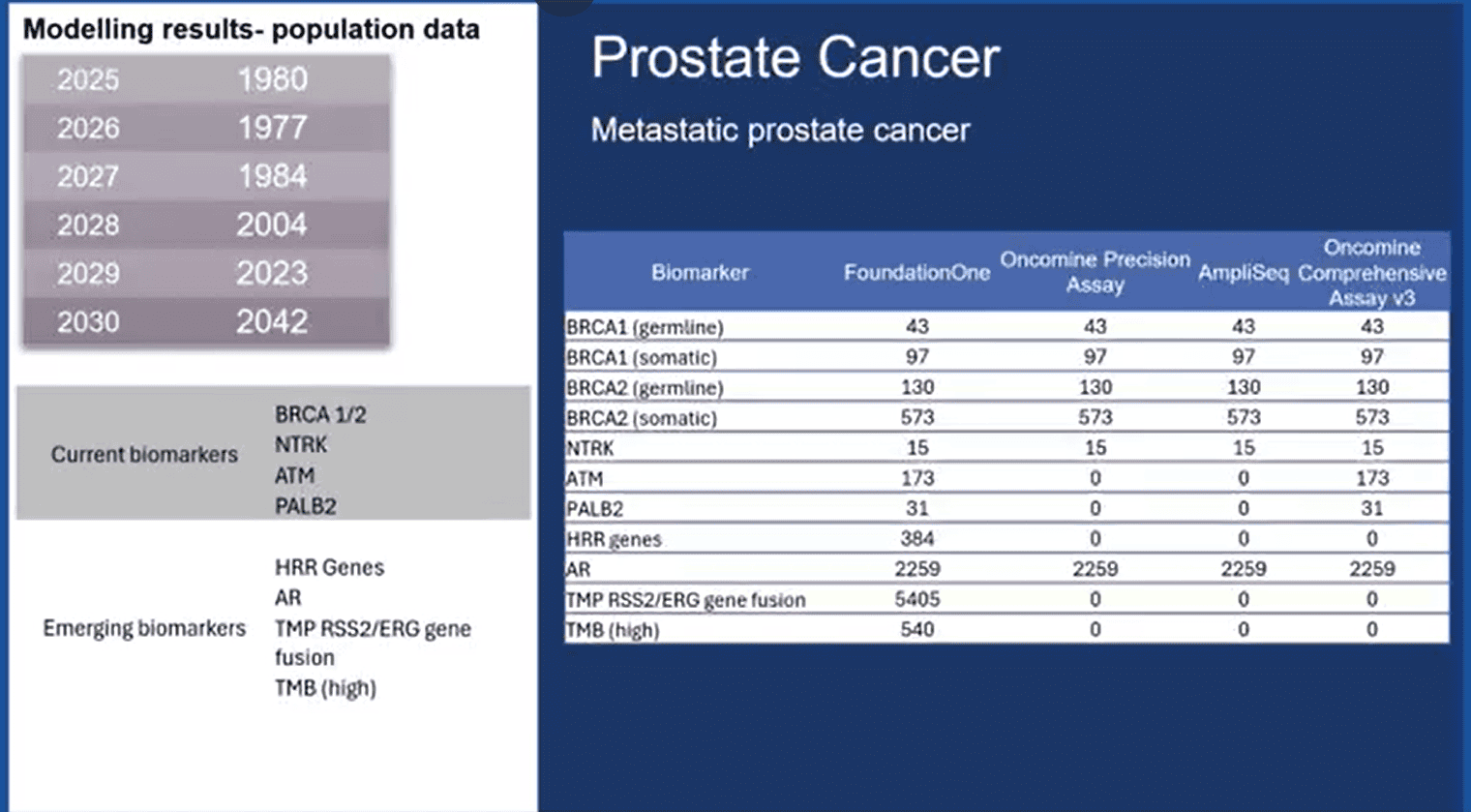
Precision Medicine is an ever-growing field and the Director of Health at the Conference Board of Canada presented data on the known vs emerging biomarkers for 5 cancers including breast, pancreatic, colorectal, prostate and lung cancer.
Breast Cancer
There are currently 4 biomarkers for breast cancer including PIK3CA, BRCA1/2, NTRK and ESR1. As for emerging biomarkers, there are 6: AKT1, PTEN, FGFR1-4, MYC, c-MET and homologous recombination repair deficiency.
Pancreatic Cancer
In terms of pancreatic cancer, there are 5 current biomarkers: BRCA1 (germline), BRCA1 (somatic), BRCA2 (germline), BRCA2 (somatic) and NTRK. As for emerging biomarkers, there are 8: PALB2, KRAS, NRAS, BRAF, NRG1, MMR/MSI, HRR genes, and TMB.
Colorectal Cancer
In the case of colorectal cancer, the number of current biomarkers is 6. They include KRAS wt, NRAS wt, BRAF wt, HER2 (non-amplified), microsatellite instability (high) and NTRK (gene fusion). The number of emerging biomarkers for colorectal cancer is also 6 and the list includes BRAF (V600 sub), HER2 (amplification), KRAT mut, c-MET (amplification), POLE (mut), and FGFR (any alteration).
Lung Cancer
Lung cancer has 6 current biomarkers which are EGFR sub./del., ALK gene fusion, ROS1 gene fusion, BRAF V600e sub., NTRK (gene fusion), and c-MET amp./fusion. As for emerging biomarkers, there are 4: RET gene fusion, KRAS mut., HER2 mut., and TMB (high).
To learn more about lung cancer biomarkers, visit this link.
Prostate Cancer
For prostate cancer, there are 4 current biomarkers: BRCA 1/2, NTRK, ATM, and PALB2. In terms of emerging biomarkers, there are 5: HRR genes, AR, TMP RSS2/ERG gene, fusion, and TMB (high).
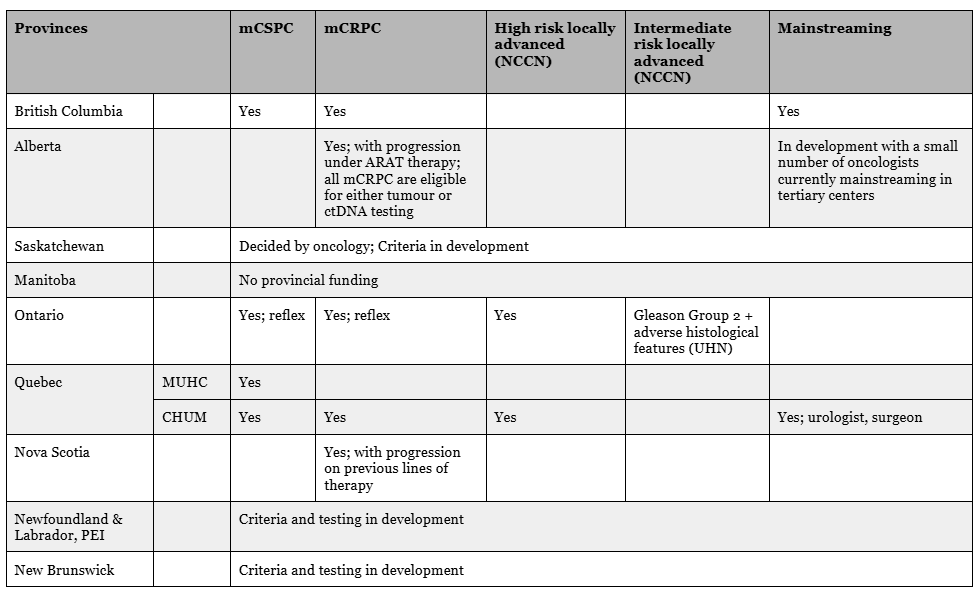
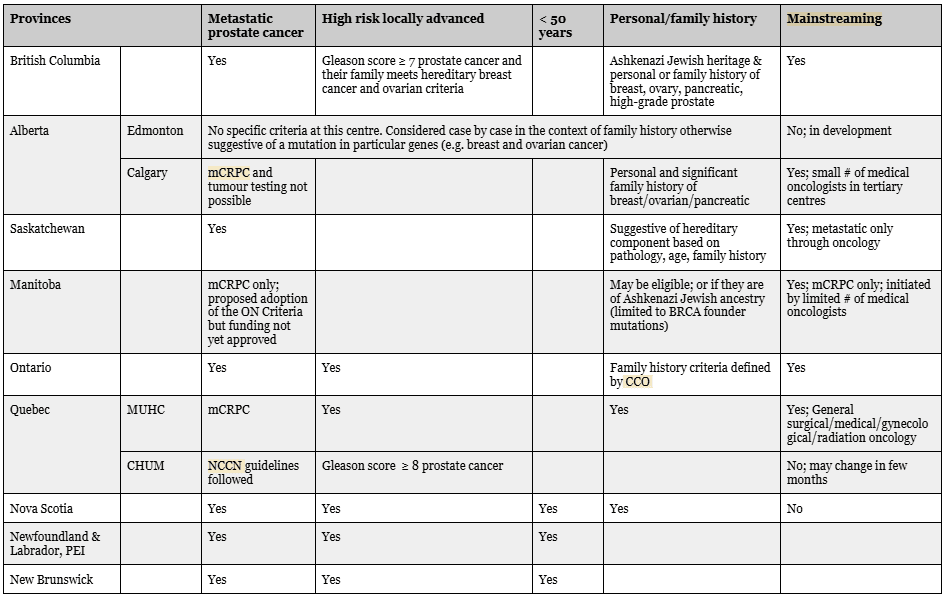
Canadian Urologist Association, Genetic Testing for Prostate Cancer
Dr. Richardo Rendon, MSc, Community Health & Epidemiology, PhD, FRCSC, Director of Research, Department of Urology, Dalhousie University
Dr. Michael Kolinsky, MD, PhD, Medical Oncologist at the Cross Cancer Institute, CCTG PR25 study chair
Dr. Shamini Selvarajah, PhD, DABMGG, FACMG, FCCMG, Assistant Professor, Department of Laboratory Medicine & Pathobiology – Cytogenetics
Below are tables outlining the tumour and genetic testing criteria for prostate cancer across Canada from the Canadian Urological Association’s (CUA) Genetic Testing for Prostate Cancer webinar.
Prostate Cancer Tumour Testing Criteria National Overview [25]
Genetic Testing Criteria for Prostate Cancer in Each Province [26]
Prostate Cancer Resources
Genetic Testing for Prostate Cancer
This website is specifically designed for prostate cancer patients who have been recently diagnosed and their families. Includes information such as an explanation of genetic testing + its significance, types of mutations, the types of genetic tests and when they are recommended, understanding your test results and frequently asked questions.
There are many misconceptions surrounding the topic of genetics and prostate cancer, this handout serves to fact-check them.
Provides information about prostate cancer screening, biomarkers, what to do after testing, genetic counselors, treatment and much more.
Study : Genes linked to aggressive prostate cancer
This resource discusses a study that looked into genes/biomarkers and their association with non-aggressive, aggressive and metastatic prostate cancer. They included many genes whose associations with prostate cancer are less commonly researched.
Prostate Cancer Risk Management
This resource explains the risks of prostate cancer and the biomarkers known to be associated with increased risk.
BRCA1/2: Why men should be screened for the “breast cancer gene”
Men carrying a BRCA1 or 2 mutation have up to an 8.6-fold increase in risk of developing prostate cancer, but not enough realize that this biomarker impacts them too. Read this to learn more about it.
Discover Essential Resources on BRCA Mutations for Men
A resource hub for men with the BRCA mutation including a FAQ Fast Facts section, Knowledge Center with detailed resources as well as other tools.
TARGET: A Genetic Education Webtool – BRCA
A self guided educational tool to make informed decisions about prostate cancer genetic testing. Includes 9 educational modules as listed below:
- Can prostate cancer be inherited?
- What is genetic testing?
- What is genetic counselling?
- Does your family history matter? What are some important family history questions to consider?
- What are the results I may get from a genetic test?
- What are the types of genetic tests? What do I need to know about the various genetic testing panels?
- How often are inherited mutations found in men with prostate cancer? Which genes have the highest risk of prostate cancer?
- Are there any risks of doing genetic testing with regards to my insurance?
- What does my genetic test mean for my family?
Prostate Cancer Genetics Podcast
This podcast discusses genetic counseling, genetic testing, and the impact of genetics in prostate cancer for patients and families, with special guest appearances such as physicians, genetic counsellors, patients and families.
Episodes include:
- What is Genetic Counselling for Prostate Cancer?
- What is Genetic Testing for Prostate Cancer?
- Patient Experience with Genetic Testing for Prostate Cancer?
- Impact of Genetic Testing for our Family
- Important Genes and Genetic Syndromes Involved in Prostate Cancer
- Precision Medicine in Prostate Cancer
BRCA1 AND BRCA2 IN MEN | Basser Center – Fact Sheet
This fact sheet covers what it means for a man to have a hereditary BRCA 1 or 2 biomarker identified, the recommended screenings that follow, etc.
BRCA Gene in Men: What it Means for Cancer Risk
This article covers the impact of the BRCA 1/2 biomarker in men; the types of cancer tied to this biomarker, when to consider getting tested for BRCA 1/2, how it gets passed down through families, the difference in cancer risk for BRCA 1 vs BRCA 2, etc.
BRCA Gene Changes: Cancer Risk and Genetic Testing Fact Sheet – NCI
The National Cancer Institute has put together a page with ten key questions about the implications of the BRCA gene/biomarker in cancer and genetic testing.
Why Men Should Consider BRCA Gene Testing
A news report including a patient story of their experience with prostate cancer caused by the BRCA gene and how genetic testing impacted them.
Cancer Risk in BRCA-Positive Men
This podcast episode covers all-things BRCA in men; associated risks of cancer, who is recommended to get screened, etc.
Genetic Testing For Prostate Cancer | BRCA | #MarkScholzMD #AlexScholz #PCRI
This interview with a 30 year medical oncologist covers the difference between genomic and genetic testing, the relevance of these in the case of prostate cancer, as well as somatic vs germline testing.
Did you know that males carrying the BRCA2 biomarker are at high risk for developing aggressive prostate cancer at an earlier age? If not, you should probably check out this resource for more information, particularly about BRCA in the Ashkenazi Jewish population who are at higher risk.
BRCA in BC’s brochure expands on how to find support, some fast facts about BRCA, as well as how and why to test for this biomarker.
Cancer Predisposition Syndromes [27]
When it comes to tumours, 75%-80% are developed throughout a person’s lifetime (sporadic) rather than passed down in their family [28]. The other 20%-25% are familial, 10%-15% of which are passed down in the genes (hereditary) while the rest could be due to similar lifestyle factors or living conditions for instance [29]. Dating back 200 years, some of the first families reported to have hereditary cancer include the family of a French physician Broca whose family had a large amount of breast cancer cases, as well as Napoleon’s family which had lots of gastric cancer[30]. Cancer predisposition syndromes tend to cause cancer at a younger age and in numerous members of a family in comparison to cancer in general [31]. They are worth identifying as this allows health practitioners to help develop risk-reducing strategies for at-risk family members and for those with cancer, guide their treatment [32]. Important to note that something can’t typically be categorized as a “syndrome” without a family history [33].
Below is a list of various cancer predisposition syndromes and the systems they affect. Information on the most commonly tested ones has been linked to their titles.
| Impacted System | Cancer Predisposition Syndromes + genes |
| Digestive |
|
| Urogenitory |
|
| Skin, Soft Tissue and Bone |
|
| Endocrine |
|
| Blood, Bone marrow and Lymphatic systems |
|
| Nervous |
|
| Immune |
|
*It’s important to note that not all of these genes can be tested for as of this point
Source: Liu, D. (2020). Handbook of Tumor Syndromes (1st ed.). CRC Press. August 11, 2025, https://www-taylorfrancis-com.libaccess.lib.mcmaster.ca/books/edit/10.1201/9781351187435/handbook-tumor-syndromes-dongyou-liu
Want to learn more about cancer predisposition syndromes? The AIRC Institute of Molecular Technology in Italy has a video that introduces the topic which can be found at this link.
CITATIONS
[1] Califf, R. M. (2018). Biomarker definitions and their applications. Experimental Biology and Medicine, 243(3), 213–221. https://doi.org/10.1177/1535370217750088
[2] Califf, R. M. (2018). Biomarker definitions and their applications. Experimental Biology and Medicine, 243(3), 213–221. https://doi.org/10.1177/1535370217750088
[3] Califf, R. M. (2018). Biomarker definitions and their applications. Experimental Biology and Medicine, 243(3), 213–221. https://doi.org/10.1177/1535370217750088
[4] Califf, R. M. (2018). Biomarker definitions and their applications. Experimental Biology and Medicine, 243(3), 213–221. https://doi.org/10.1177/1535370217750088
[5] Sarhadi, V. K., & Armengol, G. (2022). Molecular biomarkers in cancer. Biomolecules, 12(8), 1021. https://doi.org/10.3390/biom12081021
[6] National Cancer InstituteTumor Markers in Common Use Was Originally Published by National Cancer Institute. Available online: https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list (accessed on 7 of August 2025)
[7] Müller, D.; Gy?rffy, B. DNA Methylation-Based Diagnostic, Prognostic, and Predictive Biomarkers in Colorectal Cancer. Biochim. Biophys. Acta Rev. Cancer 2022, 1877, 188722.
[8] Poon, M.T.C.; Keni, S.; Vimalan, V.; Ip, C.; Smith, C.; Erridge, S.; Weir, C.J.; Brennan, P.M. Extent of MGMT Promoter Methylation Modifies the Effect of Temozolomide on Overall Survival in Patients with Glioblastoma: A Regional Cohort Study. Neurooncol. Adv. 2021, 3, vdab171
[9] Rendon, R., Kolinsky , M., & Selvarajah, S. (2023, April 26). Genetic Testing for Prostate Cancer . Canadian Urological Association. https://www.cua.org/program/16882
[10] Sarhadi, V. K., & Armengol, G. (2022). Molecular biomarkers in cancer. Biomolecules, 12(8), 1021. https://doi.org/10.3390/biom12081021
[11] Canadian Cancer Society / Société canadienne du cancer. (n.d.). Tumour marker tests. Canadian Cancer Society. https://cancer.ca/en/treatments/tests-and-procedures/tumour-marker-tests
[12] Tumor marker tests in common use. NCI. (2023, December 7). https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list
[13] Sarhadi, V. K., & Armengol, G. (2022). Molecular biomarkers in cancer. Biomolecules, 12(8), 1021. https://doi.org/10.3390/biom12081021
[14] Tumor marker tests in common use. NCI. (2023, December 7). https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list
[15] Lyle, B. (2024, October 25). New Genome BC Project seeks biomarkers for early detection of bladder cancer. Genome BC. https://www.genomebc.ca/blog/new-genome-bc-project-seeks-biomarkers-for-early-detection-of-bladder-cancer
[16] Tumor marker tests in common use. NCI. (2023, December 7). https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list
[17] Sarhadi, V. K., & Armengol, G. (2022). Molecular Biomarkers in Cancer. Biomolecules, 12(8), 1021. https://doi.org/10.3390/biom12081021
[18] Sarhadi, V. K., & Armengol, G. (2022). Molecular Biomarkers in Cancer. Biomolecules, 12(8), 1021. https://doi.org/10.3390/biom12081021
[19] Sammallahti, H.; Kokkola, A.; Rezasoltani, S.; Ghanbari, R.; Asadzadeh Aghdaei, H.; Knuutila, S.; Puolakkainen, P.; Sarhadi, V.K. Microbiota Alterations and Their Association with Oncogenomic Changes in Pancreatic Cancer Patients. Int. J. Mol. Sci. 2021, 22, 12978.
[20] Youssef, O.; Lahti, L.; Kokkola, A.; Karla, T.; Tikkanen, M.; Ehsan, H.; Carpelan-Holmström, M.; Koskensalo, S.; Böhling, T.; Rautelin, H.; et al. Stool Microbiota Composition Differs in Patients with Stomach, Colon, and Rectal Neoplasms. Dig. Dis. Sci. 2018, 63, 2950–2958.
[21] Tumor marker tests in common use. NCI. (2023, December 7). https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list
[22] Tumor marker tests in common use. NCI. (2023, December 7). https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list
[23] Tumor marker tests in common use. NCI. (2023, December 7). https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list
[24] Rendon, R., Kolinsky , M., & Selvarajah, S. (2023, April 26). Genetic Testing for Prostate Cancer . Canadian Urological Association. https://www.cua.org/program/16882
[25] Rendon, R., Kolinsky , M., & Selvarajah, S. (2023, April 26). Genetic Testing for Prostate Cancer . Canadian Urological Association. https://www.cua.org/program/16882
[26] Rendon, R., Kolinsky , M., & Selvarajah, S. (2023, April 26). Genetic Testing for Prostate Cancer . Canadian Urological Association. https://www.cua.org/program/16882
[27] Liu, D. (2020). Handbook of Tumor Syndromes (1st ed.). CRC Press. August 11, 2025, https://www-taylorfrancis-com.libaccess.lib.mcmaster.ca/books/edit/10.1201/9781351187435/handbook-tumor-syndromes-dongyou-liu
[28] Liu, D. (2020). Handbook of Tumor Syndromes (1st ed.). CRC Press. August 11, 2025, https://www-taylorfrancis-com.libaccess.lib.mcmaster.ca/books/edit/10.1201/9781351187435/handbook-tumor-syndromes-dongyou-liu
[29] Liu, D. (2020). Handbook of Tumor Syndromes (1st ed.). CRC Press. August 11, 2025, https://www-taylorfrancis-com.libaccess.lib.mcmaster.ca/books/edit/10.1201/9781351187435/handbook-tumor-syndromes-dongyou-liu
[30] Evans, D. G., & Woodward, E. R. (2023). Genetic predisposition to cancer. Medicine, 51(1), 75–79. https://doi.org/10.1016/j.mpmed.2022.10.011
[31] Liu, D. (2020). Handbook of Tumor Syndromes (1st ed.). CRC Press. August 11, 2025, https://www-taylorfrancis-com.libaccess.lib.mcmaster.ca/books/edit/10.1201/9781351187435/handbook-tumor-syndromes-dongyou-liu
[32] Evans, D. G., & Woodward, E. R. (2023). Genetic predisposition to cancer. Medicine, 51(1), 75–79. https://doi.org/10.1016/j.mpmed.2022.10.011
[33] Evans, D. G., & Woodward, E. R. (2023). Genetic predisposition to cancer. Medicine, 51(1), 75–79. https://doi.org/10.1016/j.mpmed.2022.10.011
[34] Evans, D. G., & Woodward, E. R. (2023). Genetic predisposition to cancer. Medicine, 51(1), 75–79. https://doi.org/10.1016/j.mpmed.2022.10.011
[35] Evans, D. G., & Woodward, E. R. (2023). Genetic predisposition to cancer. Medicine, 51(1), 75–79. https://doi.org/10.1016/j.mpmed.2022.10.011
[36] Evans, D. G., & Woodward, E. R. (2023). Genetic predisposition to cancer. Medicine, 51(1), 75–79. https://doi.org/10.1016/j.mpmed.2022.10.011
[37] Evans, D. G., & Woodward, E. R. (2023). Genetic predisposition to cancer. Medicine, 51(1), 75–79. https://doi.org/10.1016/j.mpmed.2022.10.011